

INTENDED USE
The immunoassay intended for the qualita nucleocapsid COVID Results are for the identification of SARS Antigen is generally detectable in Positive correlation with patient history and other diagnostic information is necessary to determine infe infection or co the definite cause of disease. Negative results do not rule out SARS used as the sole ba including infection control decisions. Negative results should be considered in the context of a patient’s recent exposures, history, and the presence of clinical signs and symptoms consistent with COVID a molecular assay, if necessary for patient management The COVID medical professionals or trained operators who are proficient in performing lateral flow tests. The non
Instructions for Use and local regulation.
SUMMARY
The novel coronaviruses is an acute respiratory infectious disease. People are generally susceptible. Currently, the patients infected by the novel coronavirus are the main source of infection; asymptomatic infected people can also be infectious Based on the current epidemiological investigation, the incubation period is 1 to 14 days, mostly 3 to 7 days. The main manifestations include fever, fatigue, and dry cough. Nasal congestion, runny nose, sore throat, myalgia and diarrhea are found
[PRINCIPLE]
The COVID immunoassay is based on the principle of the double technique. conjugated with color conjugation pad interact making antigen membrane via capillary action until the colored test line antigens are present in the negative result. should always appear if the test procedure is performed properly.
WARNINGS AND PRECAUtion
- For in vitro diagnostic use only.
- For healthcare professionals and settings.
- Do not use this For in vitro diagnostic use only
COMPOSITION
Materials Provided
- Discard the saliva collector; Cover the collection tube with the dropper tip Antigen is generally detectable in saliva during the acute phase of infection.
- 20 Test Cassettes: each cassette with desiccant in individual foil pouch onto the collection tube. Shake the collection tube more than three tim Positive results indicate the presence of viral antigens, but clinical
- 20 Extraction Reagents: ampoule containing 3 mL of extraction reagent vigorously to mix the saliva and the extraction reagent, then squeeze the correlation with patient history and other diagnostic information is necessary to determine infection status. Positive results do not rule out bacterial infection or co-infection with other viruses. The agent detected may not be the definite cause of the disease. Negative results do not rule out SARS-CoV-2 infection and should not be
- 20 Saliva Collectors
- 20 Collection tubes
- 20 Droppers
- 1 Work Station
- 1 Package Insert
Materials Required but not Provided
- Timer
STORAGE AND STABILITY
- Store as packaged in the sealed pouch at temperature (4-30℃ or 40-86℉). The kit is stable within the expiration date printed on the labeling.
- Remove the test cassette from the sealed
- Reverse the collection tube, holding the tube upright, transfer 3 drops (approximately 100μL) slowly to the specimen well (S) of the test cassette, lateral flow tests. The product may be used in any laboratory and
- Once open the pouch, the test should be used within one Prolonged then start the timer.
specimen Transport and Storage
Freshly collected specimens should be processed as soon as possible, but no later than one hour after specimen collection.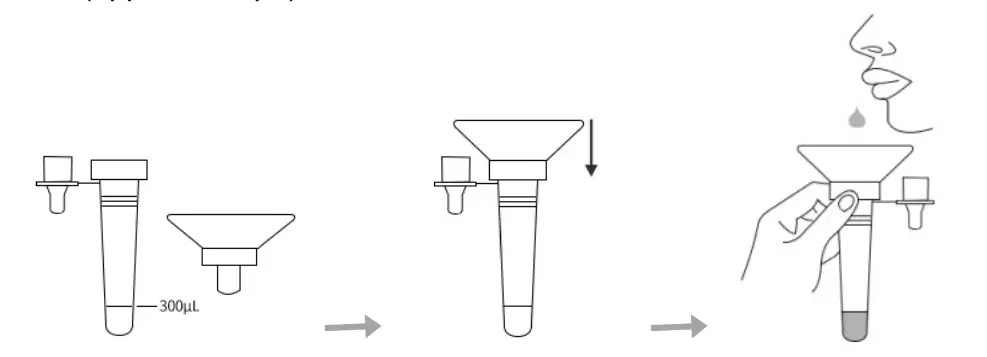
TEST PROCEDURE
Note: Allow the test cassettes, reagents, and specimens to equilibrate to room temperature (15-30℃ or 59-86℉) prior to testing.
- Place the collection tube with the saliva collector which has saliva in the work station. Unscrew the lid of an extraction reagent. Add all of the extraction reagents into the collection tube.
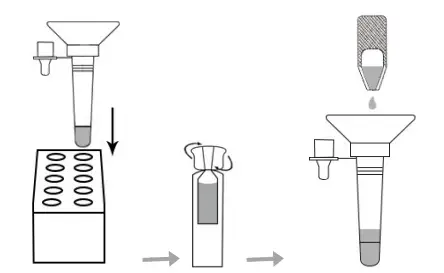
- Discard the saliva onto the vigorously to mix the saliva and the extraction mixed solution ten times to allow the saliva to be thoroughly mixed.
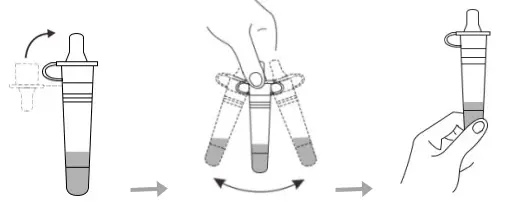
- Remove the test cassette from the sealed pouch. Reverse the (approximately 100μ then start the timer. Wait for colored lines to appear. Do not read results after 20 minutes.
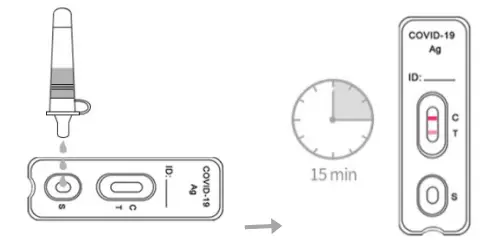
RECREATION OF RESULTS]
| Positive | Two lines appear. One colored line appears at the control region (C), and another colored line appears at the test region (T), irregard- less of the intensity of the test line. |
| N e | One colored line appears at the control region (C), and no line appears at the test region (T). |
| Invalid | Control line fails to appear. Insufficient specimen volume or incorrect procedural techniques are the most likely reasons for control line failure. Review the procedure and repeat the test using a new test cassette. If the problem persists, discontinue using the lot immediately and contact your local distributor. |
QUALITY CONTROL
A procedural control is included in the test. A colored line appearing in the control region (C) is considered an internal procedural control. It confirms sufficient specimen volume, adequate membrane wicking and correct procedural technique.
Control standards are not supplied with this kit. However, it is recommended that positive and negative controls be tested as good laboratory practice to confirm the test procedure and to verify proper test performance.
LIMITATIONS
- The product is limited to providing qualitative detection. The intensity of the test line does not necessarily correlate to the concentration of the antigen of the
- Negative results do not preclude SARS-CoV-2 infection and should not be used as the sole basis for patient management
- A physician must interpret the results in conjunction with the patient’s history, physical findings, and other diagnostic
- A negative result can occur if the quantity of SARS-CoV-2 antigens present in the specimen is below the detection threshold of the assay, or the virus has undergone minor amino acid mutation(s) in the target epitope region recognized by the monoclonal antibodies utilized in the test.
PERFORMANCE CHARACTERISTICS
Clinical Performance
The clinical performance of COVID-19 Antigen Rapid Test Cassette (Saliva) was established in prospective studies with specimens collected from 645 individual symptomatic patients (within 7 days of onset) and asymptomatic patients who were suspected of COVID-19. Summary data of COVID-19 Antigen Rapid Test as below: The RT-PCR cycle threshold (Ct) is the relevant signal value. Lower Ct value indicate higher viral load. The sensitivity was calculated for the different Ct value range (Ct value≤30 and Ct value≤37).
| COVID-19 Antigen | RT-PCR (Ct value≤30) | Total | ||
| Positive | Negative | |||
| CLUNGENE® | Positive | 120 | 2 | 122 |
| Negative | 4 | 483 | 487 | |
| Total | 124 | 485 | 609 | |
| COVID-19 Antigen | RT-PCR (Ct value≤37) | Total | ||
| Positive | Negative | |||
| CLUNGENE® | Positive | 146 | 2 | 148 |
| Negative | 14 | 483 | 497 | |
| Total | 160 | 485 | 645 | |
Limit of Detection (Analytical Sensitivity)
The study used cultured SARS-CoV-2 virus (Isolate Hong Kong/ VM20001061/2020, NR-52282), which is heat-inactivated and spiked into saliva. The Limit of Detection (LoD) is 8.6×102 TCID50/mL.
Cross-Reactivity (Analytical Specificity)
Cross-reactivity was evaluated by testing 32 commensal and pathogenic microorganisms that may be present in the oral cavity. No cross-reactivity was observed with recombinant MERS-CoV NP protein when tested at the concentration of 50 μg/mL. No cross-reactivity was observed with the following viruses when tested at the concentration of 1.0×106 PFU/mL: Influenza A (H1N1), Influenza A (H1N1pdm09), Influenza A(H3N2), Influenza B(Yamagata), Influenza B(Victoria), Adenovirus (type 1, 2, 3, 5, 7, 55), Human metapneumovirus, Parainfluenza virus (type 1, 2, 3, 4), Respiratory syncytial virus, Enterovirus, Rhinovirus, Human coronavirus 229E, Human coronavirus OC43, Human coronavirus NL63, Human coronavirus HKU1. No cross-reactivity was observed with the following bacteria when tested at the concentration of 1.0×107 CFU/mL: Mycoplasma pneumoniae, Chlamydia pneumoniae, Legionella pneumophila, Haemophilus influenzae, Streptococcus pyogenes (group A), Streptococcus pneumonia, Candida albicans,Staphylococcus aureus.
Interference
| Substance | Concentration | Substance | Concentration |
| Mucin | 2% | Whole blood Menthol Phenylephrine Histamine dihydrochloride Mupirocin Zanamivir Ribavirin Dexamethasone | 4% |
| Benzocaine | 5 mg/mL | 10 mg/mL | |
| Saline nasal spray | 15% | 15% | |
| Oxymetazoline | 15% | 10 mg/mL | |
| Tobramycin | 5 μg/mL | 10 mg/mL | |
| Oseltamivir phosphate | 10 mg/mL | 5 mg/mL | |
| Arbidol | 5 mg/mL | 5 mg/mL | |
| Fluticasone propionate | 5% | 5 mg/mL | |
| Triamcinolone | 10 mg/mL |
The following potential interference substances were evaluated with the COVID-19 Antigen Rapid Test Cassette (Saliva) at the concentrations listed below and were found not to affect test performance.
High-dose Hook Effect
The COVID-19 Antigen Rapid Test Cassette (Saliva) was tested up to 1.15×105 TCID50/mL of inactivated SARS-CoV-2 and no high-dose hook effect was observed. Hangzhou Clongene Biotech Co., Ltd. No.1 Yichuang Road, Yuhang Sub-district, Yuhang District, 311121 Hangzhou, China Shanghai International Holding Corp. GmbH (Europe) Eiffestrasse 80, D-20537 Hamburg, Germany